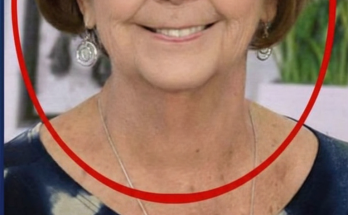
Periorbital and eyelid lesions represent a broad spectrum of dermatologic and infectious conditions. Because the ocular adnexa contain numerous sebaceous glands, sweat glands, hair follicles, and thin dermal tissue, pathologic processes in this region often present with pronounced inflammation. The image provided demonstrates significant upper eyelid edema, a central cutaneous opening with discoloration, and multiple papular and pigmented lesions distributed along the lower eyelid and malar region.
This article provides a medical-style discussion of potential etiologies, clinical implications, and recommended management strategies for similar presentations.
1. Anatomical and Pathophysiological Considerations
The eyelid is composed of:
-
Meibomian (tarsal) glands and Zeis glands, which can become obstructed or infected
-
Apocrine sweat glands (Moll glands)
-
Thin epidermal and dermal layers, susceptible to trauma and microbial invasion
-
Rich vascular and lymphatic drainage, permitting rapid spread of inflammation
Due to these features, localized glandular obstruction or minor breaches in the skin barrier may progress into acute infections or cystic formations.
2. Clinical Characteristics Observed
2.1 Upper Eyelid Lesion
The upper eyelid displays:
-
Localized erythema and swelling
-
A central opening with darkened content
-
Surrounding nodular elevations
This constellation is suggestive of an infected cyst, abscess formation, or ruptured hordeolum, though other differential diagnoses remain possible.
2.2 Periorbital Papules
Multiple small, flesh-colored papules adjacent to the eyelid margin may represent:
-
Sebaceous gland hyperplasia
-
Milia
-
Inflammatory papules associated with periocular dermatitis
2.3 Pigmented Malar Lesions
Darkened, punctate lesions over the malar region may reflect:
-
Post-inflammatory hyperpigmentation
-
Healing scabs or crusting
-
Sequelae of prior dermatologic manipulation or cosmetic procedures
The distribution pattern suggests either a reactive process or a procedure-induced cutaneous response.
3. Differential Diagnosis
Although definitive diagnosis cannot be made based on the image alone, the primary conditions that may produce similar findings include:
3.1 Hordeolum (Stye)
An acute bacterial infection—typically Staphylococcus aureus—of an eyelash follicle or associated sebaceous gland. Rupture may lead to localized abscess formation and drainage.
3.2 Chalazion With Secondary Infection
A chronic, granulomatous inflammation of the Meibomian gland. Secondary bacterial infection may create an open cavity with surrounding inflammation.
3.3 Periorbital Cellulitis or Localized Abscess
Bacterial invasion of periorbital tissues can result in erythema, warmth, tenderness, and multiple satellite lesions.
3.4 Complication of Cosmetic or Dermatologic Procedures
Procedures such as microneedling, tattooing, chemical agents, or lesion removal may lead to papular eruptions, infection, or hyperpigmented punctate marks.
3.5 Inflammatory or Allergic Dermatoses
Contact dermatitis, insect bites, or id reactions may cause grouped papules or vesiculopapular lesions.
4. Medical Significance of Periorbital Infections
Infections of the eyelid and adjacent facial structures warrant urgent evaluation because of potential progression to:
-
Preseptal or orbital cellulitis
-
Orbital abscess, requiring surgical intervention
-
Keratitis or conjunctival involvement
-
Permanent eyelid scarring
-
Vision impairment in severe cases
The periorbital region’s proximity to the orbit and brain makes prompt management essential.
5. Recommended Clinical Management
5.1 Clinical Assessment
A thorough ophthalmologic or dermatologic examination should include evaluation for:
-
Purulent drainage
-
Extension of erythema
-
Visual acuity changes
-
Extraocular muscle function
-
Lymphadenopathy
5.2 Pharmacologic Intervention
Based on the clinical diagnosis, treatment may include:
-
Topical ophthalmic antibiotics (e.g., erythromycin ointment)
-
Systemic antibiotics for suspected abscess or cellulitis
-
Warm compress therapy to promote drainage (as appropriate)
-
Topical anti-inflammatory agents for non-infectious etiologies
5.3 Procedural Treatment
When indicated, clinicians may perform:
-
Incision and drainage of abscesses
-
Sterile expression of obstructed glands
-
Removal of foreign bodies or cyst contents
5.4 Patient Counseling and Follow-Up
Patients should be advised to avoid:
-
Manipulating or squeezing lesions
-
Applying non-sterile substances
-
Using contaminated cosmetic products
Follow-up is required to ensure resolution and to monitor for complications, including orbital involvement.
6. Risk Factors and Preventive Measures
Preventive strategies include:
-
Maintaining eyelid hygiene
-
Regular removal of cosmetics
-
Avoiding expired makeup and shared applicators
-
Seeking professional care for recurrent cysts or inflammatory lesions
-
Ensuring sterility and qualifications of providers performing cosmetic procedures
7. Conclusions
Periorbital lesions, especially those accompanied by eyelid swelling and open cavities, should be evaluated promptly by a medical professional. The presentation in the provided image may correspond to a ruptured glandular infection, abscess, or dermatologic complication, but definitive diagnosis requires clinical examination. Early intervention can prevent progression to more serious ocular or orbital pathology and reduce the risk of long-term cosmetic or functional consequences.